Tools using artificial intelligence (AI) for medical imaging can help detect and classify lesions in an increasing number of clinical applications. In breast and chest imaging, algorithms can now significantly expedite workflow and improve cancer risk prediction, two experts explained during the ESR AI Premium meeting earlier this month in Barcelona, Spain.
Breast cancer screening
Breast cancer (BC) screening with mammography helps lower mortality and improves quality of life after treatment. But variability between the readings and the shortage of radiologists can be challenging for imaging performance. AI can be a wonderful ally in that respect; better than computer-aided diagnosis (CAD) could ever be, Dr. Albert Gubern-Merida, Head of Research and Development at ScreenPoint in Nijmegen, the Netherlands, told delegates during the conference. “Millions of mammograms need to be read every year that put a strain on radiology services. CAD emerged over 20 years ago to help for second readings, but the overall performance is disappointing because these systems just help the radiologist double-check things that could have been missed. Besides, those algorithms are out-dated,” he said.
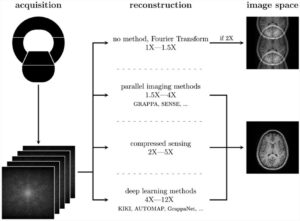
AI systems are trained on millions of images and associated data, and their performance is at least equal to radiologists, research shows. These algorithms can improve clinical performance workflow, especially in detection and decision support, according to Gubern-Merida. “AI tools can highlight things that shouldn’t be missed without interrupting the reader. AI results can simply be requested on demand when a second opinion is needed. Studies show that radiologists improve both specificity and sensitivity using these algorithms,” he said.
AI can also reduce the radiologists’ workload. BC screening with mammography requires reading a lot of images. Second reading improves detection but might be unsustainable with the introduction of Digital Breast Tomosynthesis, since the reading time increases twofold compared with 2D mammography. “Having an AI system that can help immediately differentiate between exams with and without suspicious lesions, helps save a lot of time and trouble,” he said.
Today, radiologists can already add an algorithm to their work list to sort out and label exams by their risk likelihood and divide tasks based on their work schedule.
AI could also be an option to decide when a second opinion is necessary. “Let AI decide if a second radiologist is needed to read a scan. AI systems are exceptionally good at reading normal scans, so let AI do that,” he said.
Chest applications
Computer analysis of chest radiological images is nothing new, according to Prof. Hans-Ulrich Kauczor, Chairman of Radiology and Medical Director of the Clinic of Diagnostic and Interventional Radiology at Heidelberg University. “In 1963, there were efforts to segment tumour effusion on chest x-rays. We have pursued this for a long time, but this long remained undetected by the majority of radiologists. This knowledge has only emerged in the past few years, with the leaping advances in computing power and software technologies,” he said.
Hardware and software to help segment findings and characterise lesions can now help make a huge difference in chest imaging. Chest x-ray (CXR) is the most common radiography examination worldwide. But because so many scans are being performed, thousands are not being reported in a timely manner. As a result, many findings might remain undetected when they should be, for instance, in a preoperative setting.
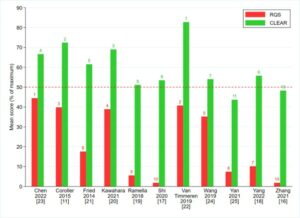
One of the major tasks for algorithms is to detect nodules. Software’s specificity and sensitivity are in the same range as an experienced radiologist’s, research shows. This reliable performance can be useful in visualising and characterising abnormalities in tuberculosis (TB) detection.
A study recently published in Computerized Medical Imaging and Graphics on lung nodule detection using deep feature fusion in chest x-ray showed that software sensitivity was 70% and specificity was up to 96% [1].
Deep learning (DL) based CAD systems can also be applied to detect pneumothorax on CXR after biopsy, with specificity around 96% and sensitivity around 90%. “In view of these good results, AI is something you can use as a concurrent reader or pre-read, or to prioritise your work,” Kauczor said.
But addressing pneumothorax or TB separately is only a minor approach, he insisted. “We would need a programme that prepares the CXR reading in a comprehensive way, to classify a scan as being normal, or having effusion or consolidations, or as being a pneumothorax.”
There are further tools out there that can analyse multiple abnormalities and findings that are easy to detect, such as normal findings, pleural effusion, consolidations, oedema and pneumothorax.
Another approach is using different training networks to aim for multiple abnormalities. Prof. Joon Beom Seo from Asan Medical Center in Seoul notably developed a method using a two-step curriculum, learning to train lesion-specified patch images and then fine-tune them with entire images that show abnormalities with different colours, depending on the findings.
Research suggests algorithms’ performance is the same as expert radiologists’, but using AI significantly reduces reading time. “AI can expedite this task. Reduced reading times are very good for workflow integration,” he said.
Software performance in CT is also very high. Systems using 3D convolutional neural networks (CNN) for automatic detection of lung nodules in chest CT offer sensitivity in the range of 95%. For picking pulmonary nodules, sensitivity is around 99%, which is a little higher than radiologists’.
It is crucial to look at the way these algorithms are being trained, Kauczor insisted. “Right now, many data sets have not been trained with diagnosis, so all of these nodules need histological proof. Any system needs to look at different data sets to predict if these nodules are benign or not. Errors exist and feedback is important; the system is learning.”
Software sensitivity is above 87% in predicting cancer risk when looking at multiple abnormalities, studies show. “That’s really an exceptional result in predicting benign and malignant nodules,” he said. Further multicentre studies showed that AI enabled to differentiate between benign vs. malignant in ca. 2,000 nodules, with a sensitivity of 92%, “something radiologists may not achieve on a routine basis.”
AI also shows very promising results in cancer prognosis or segmenting cancer stages, and beyond cancer in airway disease, COPD and emphysema.
The holy grail of chest imaging now is the ability to segment and characterise lung fibrosis, as this cannot be done by a single density-based approach. “You have to use AI or DL shaped models to find which parts are fibrotic areas in the lung that you want to characterise, and which is the lower diaphragm or other areas you don’t want to evaluate.”
[1] Wang C, Elazab A, Wu J, Hu Q (2016). Lung nodule classification using deep feature fusion in chest radiography. Comput Med Imaging Graph. 57:10-18
 Dr. Gubern-Mérida obtained his joint PhD degree in the field of medical imaging at the Diagnostic Image Analysis Group (DIAG) of the Radboud University Medical Centre in Nijmegen, the Netherlands and the University of Girona in Spain. His research focused on automated analysis of breast MRI, by developing image analysis and machine learning algorithms for breast cancer detection. As a post-doctoral researcher at DIAG, he expanded his research interest to other breast imaging modalities. In 2016, Dr. Gubern-Mérida joined ScreenPoint Medical, where he is currently the Head of Research and Development.
Dr. Gubern-Mérida obtained his joint PhD degree in the field of medical imaging at the Diagnostic Image Analysis Group (DIAG) of the Radboud University Medical Centre in Nijmegen, the Netherlands and the University of Girona in Spain. His research focused on automated analysis of breast MRI, by developing image analysis and machine learning algorithms for breast cancer detection. As a post-doctoral researcher at DIAG, he expanded his research interest to other breast imaging modalities. In 2016, Dr. Gubern-Mérida joined ScreenPoint Medical, where he is currently the Head of Research and Development.
 Prof. Hans-Ulrich Kauczor is Chairman of Radiology and Medical Director of the Clinic of Diagnostic and Interventional Radiology at Heidelberg University, and Director of the German Centre of Lung Research (DZL).
Prof. Hans-Ulrich Kauczor is Chairman of Radiology and Medical Director of the Clinic of Diagnostic and Interventional Radiology at Heidelberg University, and Director of the German Centre of Lung Research (DZL).
He studied medicine at the universities in Bonn, Heidelberg and Cologne, Germany. After having been an Associate Professor at the University of Mainz, where he previously completed his residency in radiology, he was appointed full Professor of Radiology in 2003 and led the Department of Radiology at the German Cancer Research (DKFZ) in Heidelberg.
He is especially known for his clinical and scientific work applying CT and MRI in chest disease and oncology. He notably served as President of the European Society of Thoracic Imaging, the German-Japanese Radiological Affiliation and the Fleischner Society. He also served as chair of the Research Committee and member of the Executive Council of the ESR.
Prof. Kauczor has been Chair of the Translational Lung Research Centre Heidelberg since 2008.
The lecture is available free of charge at www.mAIesr.org/recorded-lectures