Update: Listen to two experts discuss the technological progress of artificial intelligence* in healthcare: Dr. Dorin Comaniciu, PhD, Senior Vice President of Artificial Intelligence at Siemens Healthineers, and Dr. Christoph Zindel, Member of the Managing Board of Siemens Healthineers with responsibility for the Imaging and Advanced Therapies business segments, talk about the expectations of physicians, their challenges, and new opportunities to shape the future of precision medicine. Imagine that, ten years ago, the concept of artificial intelligence was still – kind of – “exotic”. Now, this has changed completely. There is an evolution underway and we’re right at the start of an exciting new era.
*AI-Pathway Companion is under development and not commercially available. Its future availability cannot be ensured.
Listen to the conversation on AI in healthcare in the player below:
In a recent interview with Dr. Dorin Comaniciu, who serves as Senior Vice President for Artificial Intelligence and Digital Innovation at Siemens Healthineers, we discussed Digital Twin Technology. This new tool could help to change the way healthcare is customised to the individual patient and utilise patient data as a preventive measure against various health issues. We talked about what costs are associated with Digital Twin Technology, how data is collected for it in order to be successful, and how the new technology will cope with the increased focus on data privacy and regulations.
What is Digital Twin Technology, and what could it mean for medicine in general and radiology in particular?
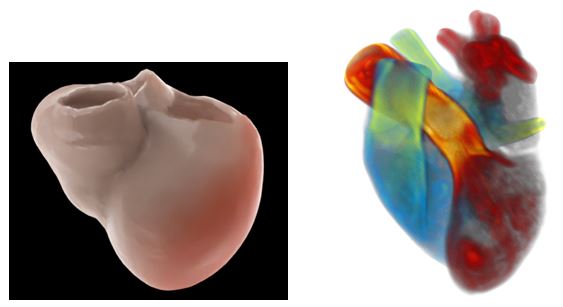
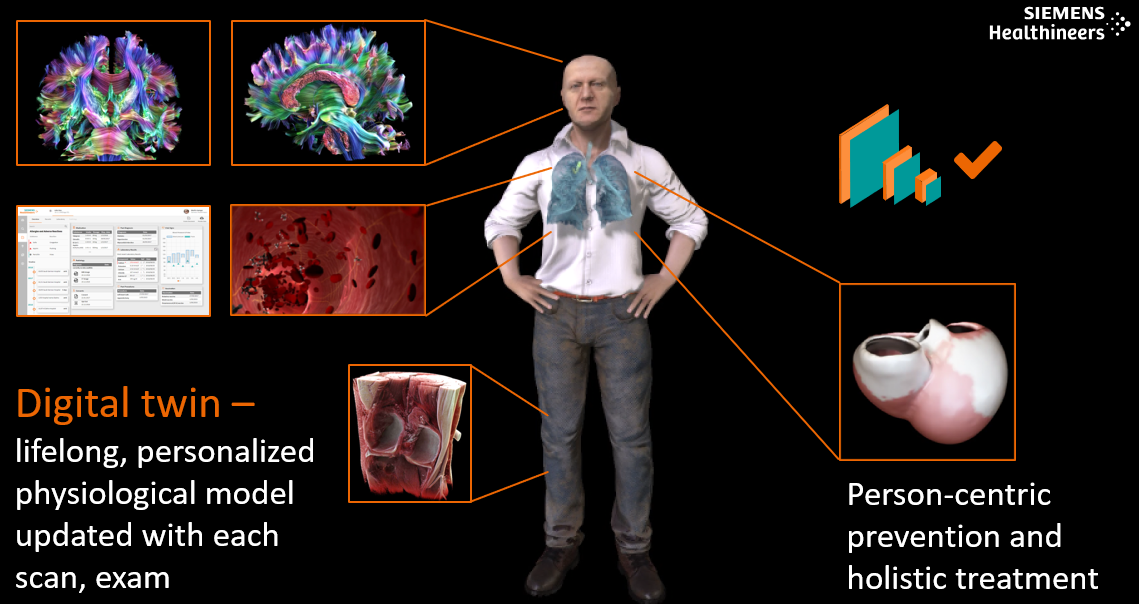
A Digital Twin is a multiscale, personalized computational model of a patient, built from the patient’s data. Imagine, for example, a model of a patient’s heart [1] built from data such as cardiac MR results, electrocardiogram results, and blood pressure readings, blood work, and genetic information using both statistical and mechanistic modelling. The model would have the same shape, dimensions, electrical signal activation, ejection fraction, and blood pressure variation as the patient’s heart. In addition, we would be able to control its functioning. It has the potential to help us virtually test and optimize treatments prior to actual treatment delivery [2].
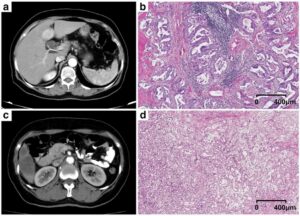
The modelling can be implemented at the organ level, such as modelling the heart, liver, or lungs; at the system level, such as the circulatory system; or at the pathology level, such as tumour growth, the mechanics of a failing knee, or the probability of a brain aneurysm rupturing. It often includes information across biological scales, from genotype to phenotype.
In radiology today, physicians often read and integrate specific data from the EMR and from images in order to derive a robust diagnosis. Digital Twin Technology [3] represents the next level of data integration – as well as providing the possibility to have a statistical view on the patient’s data, it could also supply a mechanistic model that could help to identify the next best step for the patient.
-
-
- Follow-up: What are the benefits (for both clinicians and patients)?
-
Digital Twin Technology has the potential to help clinicians expand diagnostic inference from morphology to physiology, and to support better decision-making. As for patients, they could benefit from enhanced diagnosis and personalized treatments through virtual testing and optimization of treatment prior to the actual delivery; the goal is to achieve better outcomes. For example, the Digital Twin could provide answers to the following questions: Will this patient respond to cardiac resynchronization therapy? Where and how should I ablate a liver lesion based on the thermal conductivity of the nearby vessels?
-
-
- Follow-up: What is a realistic timeframe for clinical practices to adopt Digital Twin Technology?
-
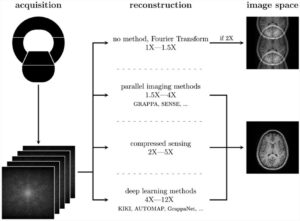
Multiple Digital Twin-like systems are currently in clinical testing. Their validation and adoption will depend on the value generated for the patient and their ease of use within the clinical workflow. Artificial intelligence [4] is an integral part of a Digital Twin since modelling begins with morphology delineation and interpretation (e.g., localization, volume and shape of the tumour, delineation of the liver vessels, liver volume and shape), which is achieved using an AI-powered inference.
How is the data necessary for training a Digital Twin acquired?
Let’s take a Digital Twin of the knee as an example. For this, one has to acquire multiple data types.
1) You need data from a cohort of patients. This information can be used to train the AI models offline that work together to build the Digital Twin. It includes contouring of the main anatomical elements of the knee and knee vicinity, such as cartilage, ligaments, bones, and muscle – and their related mechanical properties, such as the strain and stress distributions experienced by the knee structures, and the knee motion. In addition, you use outcome data to test virtual interventions or surgeries such as cartilage repair, anterior cruciate ligament reconstruction, and motion optimization.
2) Then you need data from the specific patient. This information is used to personalize the model and create the Digital Twin of the specific patient. It prepares the model for inference and treatment simulation. Note that inference could be performed before treatment to select the best option for the patient, or during treatment to optimize the delivery.
-
-
- Follow-up: How does a company or organization ethically source the data needed to train the AI systems?
-
Data can be sourced from public sources, non-profit organizations, and trusted research partners. In this context, it is important that one either operates with anonymized data or the patient explicitly consents to the use of his or her data. Depending on the regulatory bodies that govern the data source’s site and the patient, one needs to ensure that all relevant data protection regulations are complied with.
-
-
- Follow-up: Is it realistic that a single Digital Twin (e.g., heart, lungs) can exist based on a small amount of data, or does the technology require a more complete picture in order to function properly (e.g., statistics from the full-body or other organs)?
-
The databases that we use are continually growing and becoming increasingly complex and complete. In general, we focus on the smallest dataset (regarding the number of patients, data complexity, longitudinal scale) that has the desired predictive power.
In an age of concern over data privacy, what would you say to a patient or customer who is worried about their (lifelong) data being collected?
We have been working on various Digital Twin projects for cardiology, oncology, and orthopaedics for many years now. We’re making systematic progress on building and validating clinical Digital Twin systems that can bring value to patients by enabling more accurate decision making and proper treatment selection and optimization.
One line of thought is that these systems will converge into one Digital Twin for each person. The data will be integrated from birth into a lifelong, comprehensive physiological model that is updated with each scan and exam. Dedicated AI will analyze and assess the data continuously, providing specific recommendations. As a result, we don’t talk only about “disease care” but also about “health care,” person-centric prevention. And when disease happens, one has the right data and tools to make the correct diagnosis and select the best treatment.
It is perhaps too early to say how these Digital Twins will be implemented. This is due to the highly diverse nature of healthcare delivery systems: We have everything from national systems to extreme segmentation. However, a natural answer is that the Digital Twin should follow the patient, and this will be possible if the Digital Twin connection is with the patient (e.g. on his or her smartphone or wearable device).
Privacy is an important component, and the benefits of these future systems against concerns about the collection of lifelong data have to be balanced. Of course, the Digital Twin must be implemented in strict compliance with Data Privacy Law. But also, new Technology-driven privacy concepts will emerge to ensure privacy while allowing healthcare delivery to be enhanced.
Which areas of the body have the most potential when it comes to diagnosing and treating diseases by creating and applying a Digital Twin?
Many of today’s treatments have a far from ideal response rate. These include cardiac resynchronization therapy, ablation for ventricular tachycardia, tumour ablation, radiation therapy, and various orthopaedic procedures. Another area of opportunity lies in “expanding health.” How should I personalize my lifestyle to stay healthy? We are all different, and recommendations should be based on our own data. One can imagine new data acquisition programs that assess both our genotype and phenotype and integrate these into the Digital Twin in order to keep us healthy.
How accessible will Digital Twin Technology be in terms of cost and implementation?
Multiple components of Digital Twin Technology are powered by AI. This covers model building, inference, and personalization. In general, AI [4] translates into more automation and cost reduction, which implies an optimistic view. Of course, the more complex the task, the more complex the associated data and personalization procedure.
Where do you see the application of a Digital Twin regarding mobile technologies (smartphones, tablets, wearables, etc.)?
Most likely, Digital Twins will be connected to mobile technologies. Your Digital Twin would be available on your smartphone, and when you visit your physician, your data would be communicated to him or her in a digital, standardized way. Moreover, your image scan would be optimized for you in the same way.
Do you think that this technology could result in new approaches to training and educating the next generation of physicians?
Absolutely. These Digital Twin systems can potentially introduce new learning paradigms across the continuum of healthcare.
[1] https://www.siemens-healthineers.com/news/mso-solutions-for-individual-patients.html
[2] http://comaniciu.net/Papers/ModelingFailingHeart_PLoS_ONE15.pdf
[3] https://static.healthcare.siemens.com/siemens_hwem-hwem_ssxa_websites-context-root/wcm/idc/groups/public/@global/documents/download/mda5/mtmz/~edisp/siemens_healthineers_paper_embracing_healthcare_4-0-06533719.pdf
[4] https://www.siemens-healthineers.com/medical-imaging/diagnostic-imaging#AI-powered_imaging
[5] Artificial Intelligence for Computational Modeling of the Heart, T. Mansi, T. Passerini, D. Comaniciu, Academic Press, 2019
https://www.elsevier.com/books/artificial-intelligence-for-computational-modeling-of-the-heart/mansi/978-0-12-817594-1
[6] http://comaniciu.net/Papers/ModelingFailingHeart_PLoS_ONE15.pdf
 Dr. Dorin Comaniciu serves as Senior Vice President for Artificial Intelligence and Digital Innovation at Siemens Healthineers. His scientific contributions to medical imaging and machine intelligence translated into multiple clinical products focused on improving the quality of healthcare, specifically in the fields of diagnostic imaging, image-guided therapy, and precision medicine.
Dr. Dorin Comaniciu serves as Senior Vice President for Artificial Intelligence and Digital Innovation at Siemens Healthineers. His scientific contributions to medical imaging and machine intelligence translated into multiple clinical products focused on improving the quality of healthcare, specifically in the fields of diagnostic imaging, image-guided therapy, and precision medicine.
Comaniciu is a member of the National Academy of Medicine and a Fellow of IEEE, ACM, Medical Image Computing and Computer Assisted Intervention Society, and American Institute for Medical and Biological Engineering.
Comaniciu holds 300 patents and 500 patent applications in the areas of machine intelligence, medical imaging, and computer vision. He has co-authored more than 350 peer-reviewed publications, including best papers in CVPR and MICCAI, and co-wrote the book “Marginal Space Learning for Medical Image Analysis”. Furthermore, Comaniciu has recently co-authored a book in Academic Press entitled “Artificial Intelligence for Computational Modeling of the Heart” [5] and the research article “Towards Personalized Cardiology: Multi-Scale Modeling of the Failing Heart” [6].