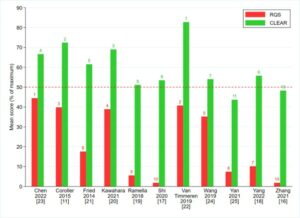
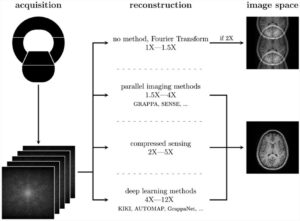
Our study included 519 screening chest radiographs (CXRs) from 294 patients enrolled in the National Lung Screening Trial (NLST) who either had proven to have lung cancer or did not have lung cancer over the duration of the trial. Five attending radiologists and three radiology residents from South Korea and the U.S. independently assessed all CXRs for the presence of lung nodules concerning for lung cancer in two sessions – first without, and then following a 4-week washout duration with help of an artificial intelligence (AI) algorithm (Lunit INSIGHT for Chest Radiography, Lunit Inc.). The AI algorithm improved the sensitivity of radiology residents for the detection of visible lung cancers which led to a greater recommendation for chest CTs (54.7% vs 70.2%, p < 0.001). For the radiologists, the AI algorithm led to improved specificity without a decrease in sensitivity for detecting lung nodules; this led to fewer chest CT recommendations (16.4% vs. 11.7%, p < 0.001) in patients without lung cancer.
Without AI aid, radiologists labelled benign findings or summation artefacts as suspicious lung nodules and requested chest CTs. AI improved their confidence and decreased the tendency of over-calling suspicious lung nodules on CXRs. As a second reader, our study shows that AI can help to both improve detection of suspicious lung nodules on CXRs and avoid “overcalling of lung nodules” and “over-recommendation of chest CTs”. Further studies will be needed to define if such improved detection of visible lung cancer on CXRs with AI algorithms can help enhance the use and improve the accuracy of CXRs in lung cancer screening.
Key points
- Reader study in the NLST dataset shows that AI algorithm had sensitivity benefit for residents and specificity benefit for radiologists for the detection of visible lung cancer.
- With AI, radiology residents were able to recommend more chest CT examinations (54.7% vs 70.2%, p < 0.001) for patients with visible lung cancer.
- With AI, radiologists recommended significantly less proportion of unnecessary chest CT examinations (16.4% vs. 11.7%, p < 0.001) in cancer-negative patients.
Authors: Hyunsuk Yoo, Sang Hyup Lee, Chiara Daniela Arru, Ruhani Doda Khera, Ramandeep Singh, Sean Siebert, Dohoon Kim, Yuna Lee, Ju Hyun Park, Hye Joung Eom, Subba R. Digumarthy & Mannudeep K. Kalra