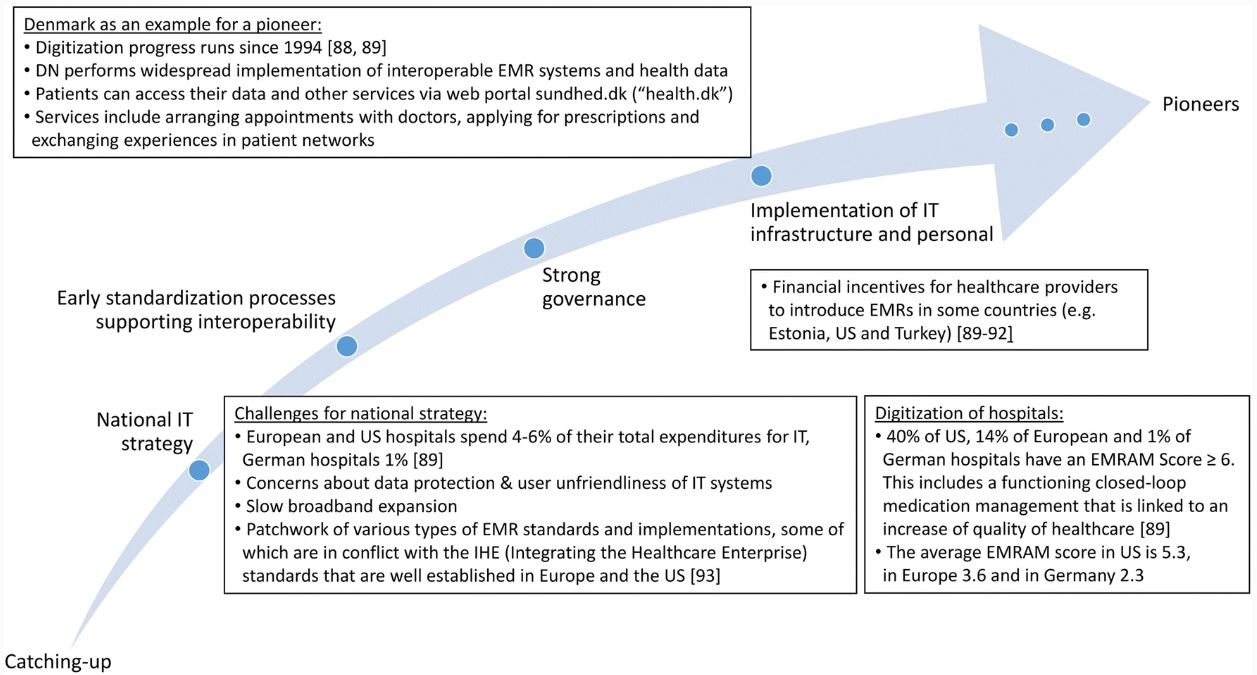
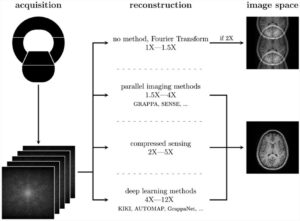
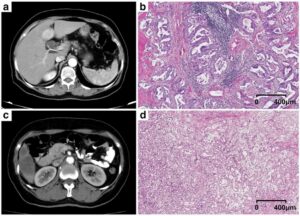
Increasing numbers of publications document the potential of radiomics and artificial intelligence (AI)-aided diagnostics, and the Corona pandemic made the importance of digitally well-connected health systems even clearer. However, although the essential technologies are already available, the progress into clinical routine application is considerably slow.
Thus, we intended to perform a comprehensive analysis to learn from the experiences of pioneering sites and countries and tried to identify the main tasks for a better clinical implementation. In a nutshell, the following challenges became apparent: a) the defensive and territorial mindset of medical disciplines with only moderate willingness to share data; b) the non-consumer-friendliness of many IT tools that increases rather than decreases the workload for the medical personnel; c) the heterogeneity of medical routine data and the difficulties in their integration making them unsuitable for training AI algorithms; d) the if at all, only partial, realization of electronic patient records; and, e) the increasing concerns about privacy protection with an uncertain legal situation.
Furthermore, approval processes for AI-based software are often unclear, and for many types of medical data, the documentation standards have not yet been defined precisely enough. Another obstacle is that in many countries funding was mostly available for research tasks on data analysis but considerably low amounts of money were spent in building the required IT infrastructures for data integration. Indeed, the latter may rather be an implementation task, which is time-consuming and costly; however, it will form the essential backbone of any clinically functionalizing system.
Thus, if we not only aim at writing appealing publications about radiomics and comprehensive diagnostics but at a digital renovation of our health systems, we need to change our mindset and convince our authorities to implement the required IT infrastructure. In this context, we also need to educate more IT-specialists to help us with the implementation and who will be important partners to keep the digital medical infrastructure running effectively. You may ask where the money should come from. Certainly, significant investments are required in the short term. However, some sites have already demonstrated that once successfully implemented, digitalized medicine will save costs in the health system and reduce administrative workload, thus giving physicians more time for their patients.
Key points
- Europe is characterized by heterogeneity in its digitization progress with predominantly national efforts. Infrastructural prerequisites for comprehensive diagnostics are not given and not sufficiently funded throughout Europe, which is particularly true for data integration.
- The clinical establishment of comprehensive diagnostics demands for a clear governance, significant investments, and cooperation at various levels in the healthcare systems.
- While comprehensive diagnostics is on its way, concerted efforts should be taken in Europe to get consensus concerning interoperability and standards, security, and privacy as well as ethical and legal concerns.
Authors: Mark Bukowski, Robert Farkas, Oya Beyan, Lorna Moll, Horst Hahn, Fabian Kiessling & Thomas Schmitz-Rode